Ncp for low platelet count – Low platelet count, or thrombocytopenia, is a condition in which the body does not have enough platelets to function properly. Platelets are essential for blood clotting, and a low platelet count can lead to excessive bleeding and bruising.
This comprehensive guide will explore the causes, diagnosis, and treatment of low platelet count, providing you with the knowledge you need to manage this condition effectively.
Pathophysiology of Low Platelet Count
Platelets, also known as thrombocytes, play a crucial role in hemostasis, the process that stops bleeding. They are small, disk-shaped cells produced in the bone marrow and have a lifespan of approximately 10 days. When a blood vessel is damaged, platelets aggregate at the site of injury, forming a plug that prevents excessive blood loss.
Thrombocytopenia, or a low platelet count, can occur due to various factors. One common cause is increased platelet destruction, which can result from conditions such as immune thrombocytopenia purpura (ITP), where the immune system mistakenly attacks platelets, or thrombotic thrombocytopenic purpura (TTP), a rare disorder characterized by the formation of blood clots in small blood vessels.
Causes of Thrombocytopenia, Ncp for low platelet count
- Increased Platelet Destruction:
- Immune thrombocytopenia purpura (ITP)
- Thrombotic thrombocytopenic purpura (TTP)
- Disseminated intravascular coagulation (DIC)
- Decreased Platelet Production:
- Bone marrow failure syndromes
- Aplastic anemia
- Leukemia
- Sequestration of Platelets:
- Splenomegaly (enlarged spleen)
- Hypersplenism
Diagnosis of Low Platelet Count

Diagnosing thrombocytopenia involves a comprehensive evaluation of clinical symptoms and laboratory tests to determine the underlying cause. The clinical presentation can provide valuable clues, while laboratory tests confirm the platelet count and help rule out other potential conditions.
Clinical Presentation
Individuals with thrombocytopenia may experience a range of symptoms depending on the severity of the condition. Common clinical manifestations include:
- Easy bruising or excessive bleeding from minor cuts or injuries
- Nosebleeds or bleeding gums
- Heavy or prolonged menstrual bleeding
- Skin rashes or petechiae (small, pinpoint-sized red or purple spots on the skin)
li>Fatigue or weakness due to blood loss
Laboratory Tests
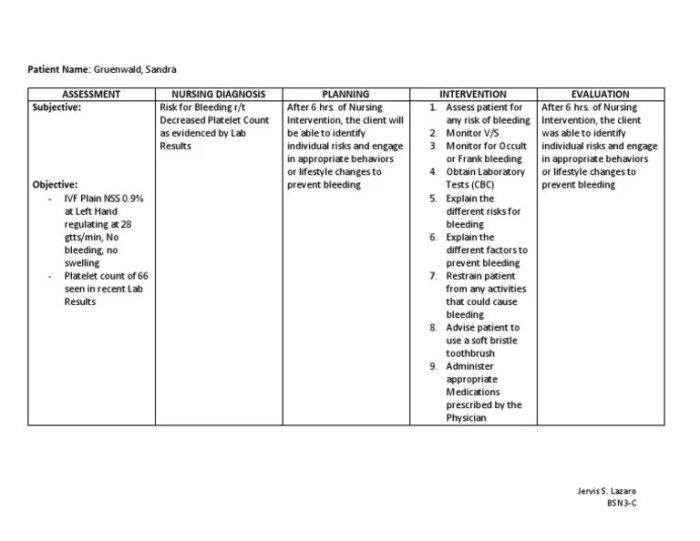
Confirming thrombocytopenia requires a complete blood count (CBC), which measures the number of platelets in a blood sample. A platelet count below 150,000 platelets per microliter (µL) is considered thrombocytopenia.
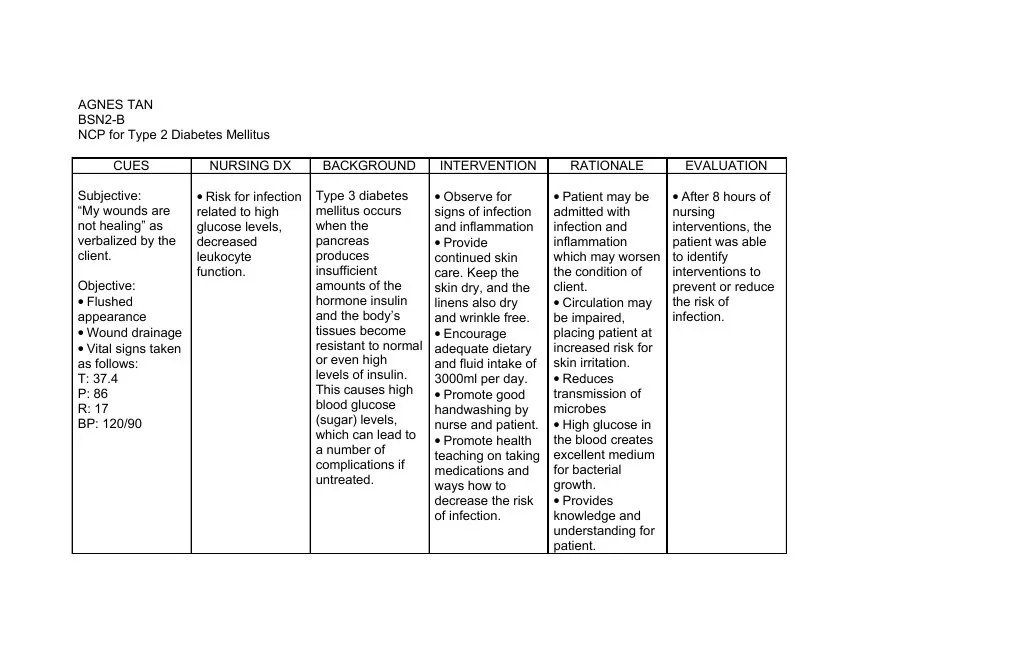
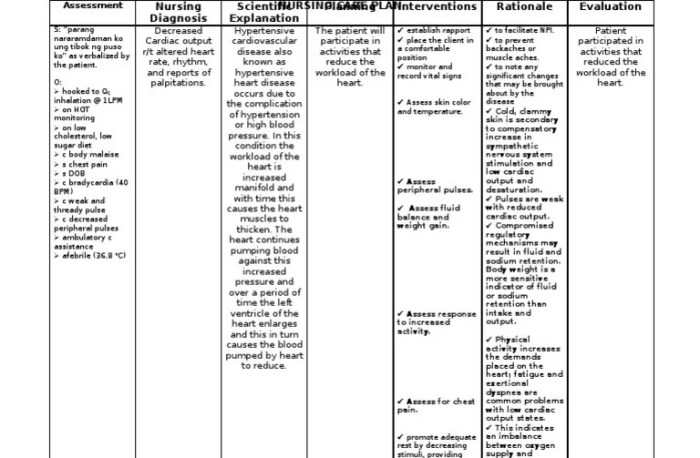
To address low platelet counts, nurses can implement nursing care plans (NCPs) that include measures to monitor and manage the condition. For further insights into complex scientific concepts, you may refer to resources like the gizmo sled wars answer key . Returning to the topic of NCPs for low platelet counts, it’s crucial to assess the patient’s history, monitor vital signs, and provide education on potential complications.
Additional laboratory tests may be performed to assess the function of platelets and identify the underlying cause. These tests may include:
- Platelet aggregation studies: These tests measure the ability of platelets to clump together and form clots.
- Bleeding time: This test evaluates the time it takes for a small cut to stop bleeding, which can provide insights into platelet function.
- Bone marrow biopsy: In some cases, a bone marrow biopsy may be necessary to determine if the low platelet count is due to a problem with platelet production.
Importance of Differential Diagnosis
Differentiating thrombocytopenia from other conditions is crucial to determine the appropriate treatment plan. Conditions that can mimic thrombocytopenia include:
- Pseudothrombocytopenia: A condition in which the platelet count appears low due to laboratory artifacts, not a true decrease in platelet production.
- Thrombocytopathy: A condition in which platelets are present but do not function properly.
- Leukemia: A type of cancer that can affect the production of platelets in the bone marrow.
Treatment of Low Platelet Count
The treatment approach for thrombocytopenia depends on the underlying cause and the severity of the condition. Treatment options may include:
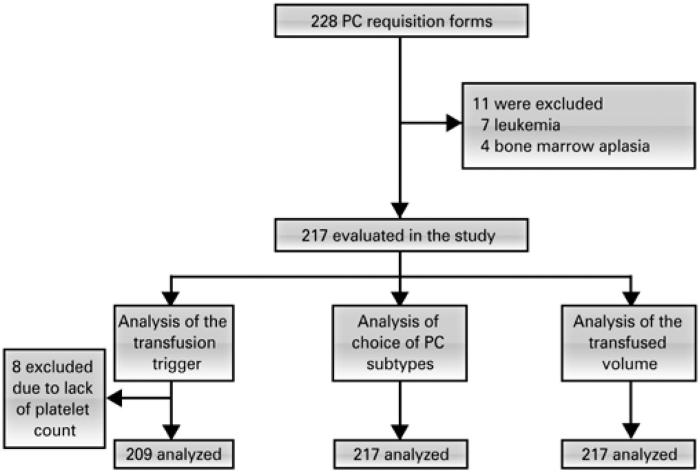
Platelet Transfusions
Platelet transfusions are the primary treatment for severe thrombocytopenia. Platelets are blood components that help stop bleeding. During a platelet transfusion, platelets are transfused into the bloodstream to increase the platelet count and reduce the risk of bleeding.
Prevention of Low Platelet Count: Ncp For Low Platelet Count
Maintaining a healthy platelet count is crucial for overall well-being. By understanding the modifiable risk factors and implementing preventive measures, we can effectively reduce the chances of developing thrombocytopenia.
Modifiable risk factors for thrombocytopenia include certain medications, infections, and lifestyle choices. It is important to consult with a healthcare professional to determine the underlying cause and discuss appropriate preventive strategies.
Medications
Certain medications, such as chemotherapy drugs and antibiotics, can cause a temporary decrease in platelet count. It is essential to discuss alternative treatment options or dosage adjustments with your doctor if thrombocytopenia is a concern.
Infections
Viral and bacterial infections can trigger thrombocytopenia. Practicing good hygiene, getting vaccinated, and seeking prompt medical attention for infections can help prevent platelet count reduction.
Lifestyle Choices
Excessive alcohol consumption and smoking can contribute to low platelet count. Limiting alcohol intake and quitting smoking can significantly improve platelet production.
Vaccination and Infection Control
Vaccinations against common infections, such as measles, mumps, and rubella (MMR), can help prevent thrombocytopenia caused by these diseases. Additionally, practicing good hygiene, including regular handwashing and avoiding contact with sick individuals, can reduce the risk of infections that may lead to thrombocytopenia.
Frequently Asked Questions
What are the common causes of low platelet count?
Common causes include immune disorders, infections, medications, and certain medical conditions such as leukemia and aplastic anemia.
How is low platelet count diagnosed?
Diagnosis involves a physical examination, blood tests to measure platelet count, and other tests to identify the underlying cause.
What are the treatment options for low platelet count?
Treatment depends on the cause and severity of the condition. Options include platelet transfusions, medications to stimulate platelet production, and addressing the underlying cause.